Myalgia and Succinylcholine
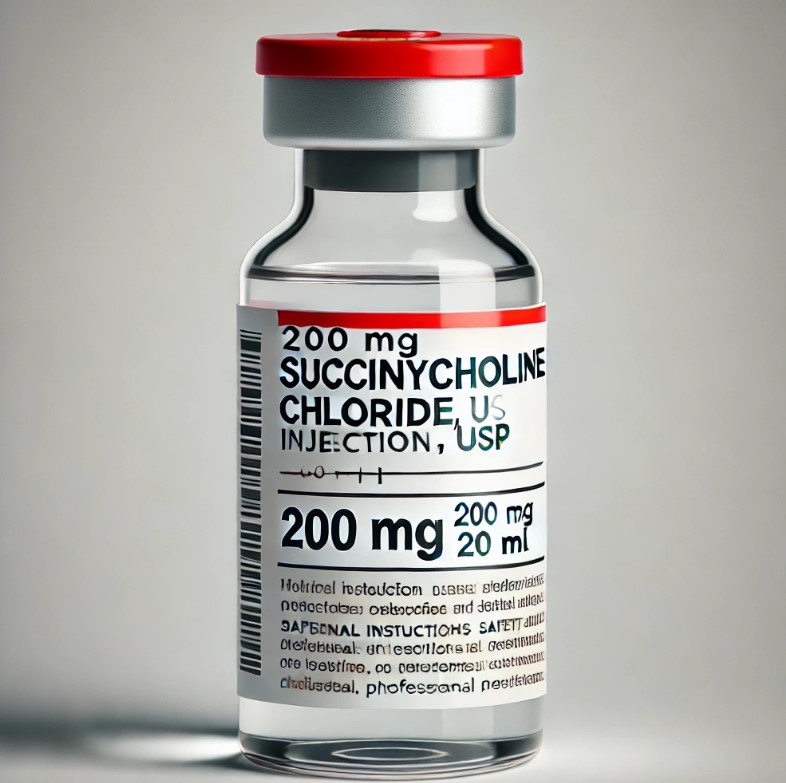
Succinylcholine is a widely used neuromuscular blocking agent in anesthesia, valued for its rapid onset and short duration of action. It has historically been the agent of choice for facilitating endotracheal intubation during general anesthesia and in emergency situations requiring rapid airway management. However, despite its clinical advantages, succinylcholine is associated with several side effects, including postoperative myalgia (POM).
Postoperative myalgia (muscle pain) following succinylcholine administration was first described in the medical literature in 1952. Since then, it has been a subject of extensive research and clinical observation. The incidence of succinylcholine-induced myalgia varies widely, with reports ranging from 1.5% to as high as 90% of patients receiving the drug. This wide range likely reflects differences in study methodologies, patient populations, and definitions of myalgia used in various research efforts. However, a generally accepted estimate places the incidence at around 50%.
The clinical presentation of succinylcholine-induced myalgia can vary in severity and duration. Patients typically describe the pain as similar to that experienced after intense physical exercise. The discomfort often begins within 24 hours after surgery and can persist for several days. In most cases, the myalgia is self-limiting and resolves without specific treatment. However, in some instances, the pain can be severe enough to interfere with a patient’s return to normal activities, including work or school.
The exact pathophysiology of succinylcholine-induced myalgia remains incompletely understood, but several theories have been proposed. The most widely accepted explanation relates to the fasciculations observed immediately after succinylcholine administration. These fasciculations, which are visible muscle twitches, are thought to result from the initial depolarization of muscle fibers caused by succinylcholine. The unsynchronized contractions of muscle fibers during fasciculations may lead to shearing forces within the muscle, causing microscopic damage to muscle fibers and their surrounding connective tissue.
Interestingly, the severity of visible fasciculations does not always correlate with the intensity of subsequent myalgia. This observation has led researchers to explore other potential mechanisms, including changes in muscle membrane permeability, release of intracellular contents, and alterations in local electrolyte concentrations. Some studies have also investigated the possibility of an inflammatory component, although current evidence suggests that inflammation may not play a significant role in the development of succinylcholine-induced myalgia.
Given the frequency and potential impact of succinylcholine-induced myalgia, numerous strategies have been investigated to prevent or reduce its occurrence. The most commonly employed technique is the administration of a small dose of a non-depolarizing neuromuscular blocking agent 2-3 minutes before succinylcholine. This technique has shown effectiveness in reducing the incidence and severity of myalgia. However, it may delay the onset of succinylcholine’s action and increase the dose requirements, making it less suitable for emergency situations.
Other pharmacological interventions that have shown some efficacy in preventing succinylcholine-induced myalgia include the use of nonsteroidal anti-inflammatory drugs (NSAIDs), lidocaine, and magnesium. A meta-analysis by Schreiber et al. found that NSAIDs were among the most effective agents for preventing myalgia, with lidocaine and rocuronium also found to be effective.
Despite these preventive strategies, it’s important to note that many of them introduce their own set of potential side effects and considerations. For example, the use of non-depolarizing neuromuscular blocking agents carries a dose-dependent risk of adverse effects such as blurred vision, diplopia, voice disorders, and difficulty in breathing and swallowing.
While succinylcholine remains a valuable tool in anesthesia practice in some settings, particularly for rapid sequence induction and short surgical procedures, the risk of postoperative myalgia is a significant consideration. When available, many physicians argue for rocuronium as an alternative, non-depolarizing neuromuscular blocking agent with rapid onset. For internists and other non-anesthesia providers, recognizing succinylcholine-induced myalgia as a potential cause of postoperative muscle pain can help avoid unnecessary investigations and interventions. As research continues, a better understanding of the underlying mechanisms and more targeted preventive strategies may emerge, further improving patient comfort and satisfaction in the perioperative period.
References
1. Wong SF, Chung F. Succinylcholine‐associated postoperative myalgia. Anaesthesia. 2000;55(2):144-152.
2. Ha N, Griffith S. A case of succinylcholine-induced postoperative myalgia. Providence St. Joseph Health Digital Commons. 2021.
3. Pandey CK, Tripathi M, Joshi G, Karna ST, Singh N, Singh PK. Prophylactic use of gabapentin for prevention of succinylcholine-induced fasciculation and myalgia: a randomized, double-blinded, placebo-controlled study. J Postgrad Med. 2012;58(1):19-22.
4. Schreiber JU, Lysakowski C, Fuchs-Buder T, Tramèr MR. Prevention of succinylcholine-induced fasciculation and myalgia: a meta-analysis of randomized trials. Anesthesiology. 2005;103(4):877-884.
5. Yun MJ, Kim YH, Go YK, et al. Remifentanil attenuates muscle fasciculations by succinylcholine. Yonsei Med J. 2010;51(4):585-589.
