What is an Epidurogram?
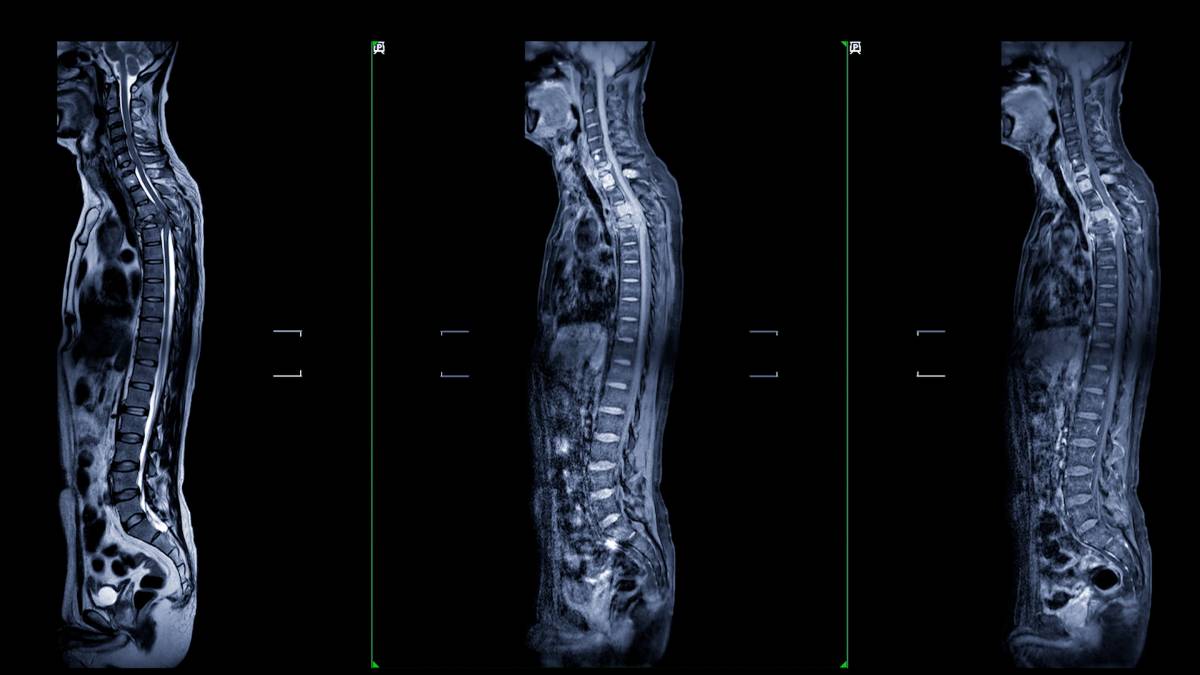
Epidural injections—injections of medication into the epidural space of the spine—are used in several contexts in medicine. For example, epidural glucocorticoid injections have long been utilized for managing pain in patients suffering from radiculopathy, spinal stenosis, and nonspecific low back pain. A needle is inserted between the ligamentum flavum and the dura. An epidural injection can be carried out through various approaches, including the translaminar, transforaminal, or caudal routes, and is typically performed by specialized medical professionals like anesthesiologists, physiatrists, or interventional radiologists. Accurate delivery of the medication to the intended site is critical for efficacy and safety. Physicians may use an epidurogram to visualize the target site and improve injection accuracy.
Traditionally, epidural injections were done using a blind technique without real-time imaging guidance. Though proper training greatly reduces risk, it is still possible to have incorrect needle placement and inadvertent injection into unintended areas such as the subarachnoid space. Studies have shown that even skilled practitioners had inaccurate needle placement rates of 25% to 30% with blind techniques, leading to concerns regarding safety and efficacy. The potential complications of misplacement, including adhesive arachnoiditis, underscore the importance of accurate delivery.
In response to these concerns, there has been an increase in the usage of fluoroscopic guidance and an epidurogram, which involves injecting contrast material under fluoroscopy to visualize the epidural space before administering the medication. This approach significantly reduces the risk of misplacement and associated complications. It allows practitioners to confirm accurate needle placement within the epidural space, minimizing the risk of intrathecal injections and their potential consequences.
The epidurogram has improved the safety and efficacy of epidural injections. By visualizing the dispersion of contrast dye, practitioners can ensure the needle is correctly positioned in the epidural space. Understanding the patterns of contrast spread after obtaining images is essential in determining the placement of an epidural catheter. In the epidural space, the dye should spread circumferentially and along nerve sheaths, creating a ‘wraparound’ pattern, or partially disperse in a ‘honeycomb’ pattern within epidural fat. Malpositioned catheters in the subdural or subarachnoid spaces show different patterns. Subarachnoid injections fill the intrathecal space extensively, while subdural injections only opacify dural margins.
While an epidurogram is generally safe, there are potential side effects, including facial flushing, low-grade fevers, hiccups, insomnia, headaches, water retention, increased appetite, increased heart rate, and abdominal cramping or bloating. However, these side effects are rare and typically resolve within a few days.
Epidural injections are a valuable tool for managing pain in patients in certain situations. The use of fluoroscopic guidance and an epidurogram has significantly improved the safety and efficacy of these injections, ensuring accurate delivery of medications to the intended site and minimizing the risk of complications.
References
Du Pen SL, Williams AR, Feldman RK. Epidurograms in the management of patients with long-term epidural catheters. Reg Anesth. 1996 Jan-Feb;21(1):61-7. PMID: 8826026.
Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976). 1987 Apr;12(3):264-8. doi: 10.1097/00007632-198704000-00013. PMID: 2954221.
Cassidy JD, Carroll LJ, Côté P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998 Sep 1;23(17):1860-6; discussion 1867. doi: 10.1097/00007632-199809010-00012. PMID: 9762743.
Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. BMJ. 1998 May 2;316(7141):1356-9. doi: 10.1136/bmj.316.7141.1356. PMID: 9563990; PMCID: PMC28536.
Van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine (Phila Pa 1976). 1997 Feb 15;22(4):427-34. doi: 10.1097/00007632-199702150-00015. PMID: 9055372.
Pengel LH, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis. BMJ. 2003 Aug 9;327(7410):323. doi: 10.1136/bmj.327.7410.323. PMID: 12907487; PMCID: PMC169642.
Pengel HM, Maher CG, Refshauge KM. Systematic review of conservative interventions for subacute low back pain. Clin Rehabil. 2002 Dec;16(8):811-20. doi: 10.1191/0269215502cr562oa. PMID: 12501942.
Vroomen PC, de Krom MC, Slofstra PD, Knottnerus JA. Conservative treatment of sciatica: a systematic review. J Spinal Disord. 2000 Dec;13(6):463-9. doi: 10.1097/00002517-200012000-00001. PMID: 11132976.
